Is taking medication for depression the ‘easy option?’ I come across this viewpoint regularly on social media. Usually there is a suggestion alongside that therapy, which I completely agree is hard work, is somehow a purer way to recover. The right way.
The history of psychiatry is rich in references to morality. Is a person ‘mad’ or ‘bad’? Is there really something wrong in the brains of those society labels as bad? Is addiction an illness or simply a behaviour choice? Are we excusing bad behaviour by medicalising it?
Many people who consider medication for depression will find themselves wondering whether it is a ‘good’ thing to take it. When you are depressed it can be very difficult to decide what is the best thing to do, and decisions are taken not only on the basis of discussion with health professionals- moral judgments also play an important part.
- How does taking antidepressants affect how I feel about me? Does it mean that I am weak?
- Is it the easy option?
- Shouldn’t I be able to sort myself out without them?
- What will other people think- my family- my friends…will it change how they see me?
Alice Malpass and her colleagues identified two parallel journeys that the depressed person embarks on. The ‘medical’ journey goes something like this:
- I have a duty to be well. Other people need me to be well.
- If I recover then there won’t be any risk of being seen as ‘mentally ill’.
- I can get back to my old self and be in charge of my life again.
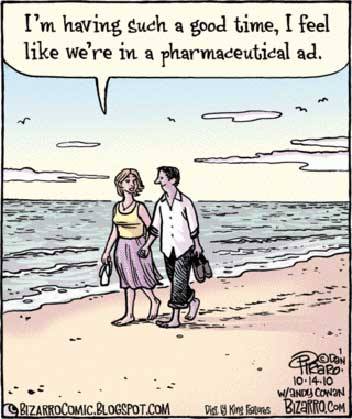
I’m sure I’ve used some of these arguments in conversation with patients. Any doctor who says they haven’t is not telling the truth- but to consider these are the only things of concern about medication is inherently simplistic and paternal, and reminds me of the cartoon of a couple walking along a beach, smiling and carefree, who say they feel so good they must be in a pharma advert.
In parallel the person is perhaps also on another journey- the ‘moral’ one.
- I feel awful because I have to ask for help.
- I feel even worse because I need to take tablets.
- Is this person the real, authentic me? Am I now my old self or someone else? Or am I only this person because I am on tablets?
- Am I hooked on these now?
Damien Ridge, who has analysed many interviews with people who are depressed talks not only about the lack of legitimacy for tablets, but also for what they are being prescribed for.
- Is ‘depression’ real?
- Shouldn’t I just ‘pull myself together’? Isn’t that what everyone else thinks?
There is a great deal of literature on whether ‘depression’ is ‘real’ or simply no more than unhappiness. And if it isn’t real, then the treatment for it cannot be legitimate either, little better than using street drugs- as one person in Ridge’s paper calls his tablets: ‘My dirty little habit’. I’ve spent my career arguing that to use the term depression is not simply medicalising misery but giving a name to a particular experience and quality of suffering which is not just unhappiness but a deep, dark, hopeless, despair. It has many causes, and it isn’t a single ‘phenomenon’ whatever DSM tells us. But it’s a state of mind that many people with different stories share in common. I experience it too. I have asked all of these questions of myself. I have watched colleagues who work in mental health look a little embarrassed when I get out the tablets at breakfast. Perhaps I do that simply to show I am not ashamed- but I do wish I could have lived my life without them.
All of the above supposes that antidepressants do actually work. Many people think they don’t, and others think they can do harm. You can find my views on these points elsewhere on this blog. I take them myself and they keep me reasonably well, but I have friends and colleagues for whom they have not worked- the medical journey is inherently optimistic- just like the pharma ads, but in reality life is far more complicated. And they are never sufficient on their own.
If doctors, and sometimes friends and family, try and influence you to focus on the ‘medical journey’ then others will try to steer your moral journey. It is really hard to focus on what is right for you when you cannot think clearly. When you are depressed, you are already struggling with guilt and shame and sometimes that can tragically end with the decision that the world is better off without you- that this is the right thing to do.
So I would only ask those who make even subtle comparisons between the easy way to ‘block out the pain’ with meds and the hard way of suffering through therapy to think before they write. It is only human to want to alleviate pain, and sometimes the tablets are the only thing that will do it. To infer that a person needs to suffer in order to be blessed is one of the ultimate moral judgments- and can be found in most religions.
Depressed or not, clinician or service user, expert or lay person-none of us have the right to sit in judgment over others.
My memoir: The Other Side of Silence: A Psychiatrist’s Memoir of Depression is available now.